



A blastocyst is an embryo that consists of more than 100 cells and forms 5 days after fertilization.
Using sophisticated culture media, we can select embryos that remain healthy in culture and reach the blastocyst stage prior to transfer.
A higher implantation rate has been observed following transfer of blastocysts. Currently our practice is to transfer 1 to 2 embryos at blastocyst stage.
The extra embryos are then frozen by vitrification. In case of less number of good quality embryos, a Day 3 transfer of 2 embryos can be performed.

It is a technique used for egg & embryo freezing by vitrification. Allows rapid cooling of cells with liquid nitrogen and does not allow crystal formation
Preferred in cases :
At risk of OHSS
With surplus embryos
Fertility preservation
Going for PGT/PGS
Previous failed fresh embryo transfer
Donor egg/embryo tarnsfer
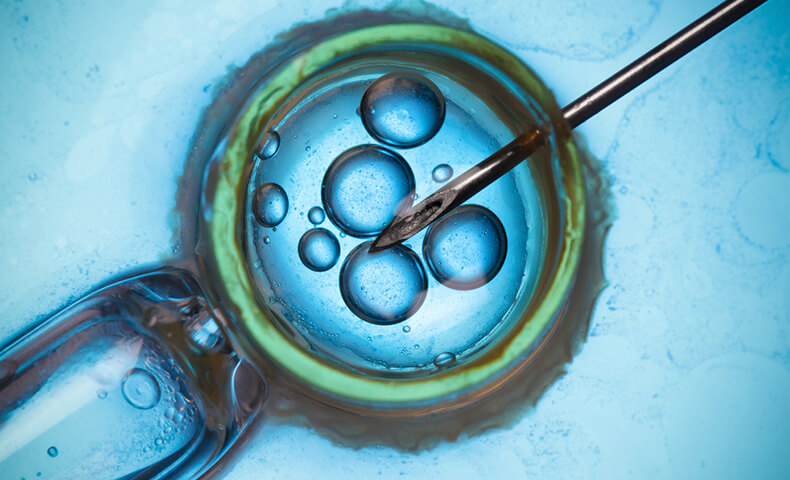
Prior to implantation, the embryo has to escape out of its protective shell known as the zona pellucida by a process known as hatching.
If this process is not completed properly, implantation will fail and pregnancy will not occur. Laser technology for Assisted Hatching (LAH), where a laser beam is focused over the zona pellucida making a small opening, to facilitate embryo hatching.
This is particularly useful for older women (more than 35 years), women with oocytes showing a thick zona and women who have tried IVF unsuccessfully.
Laser Assisted Hatching is also carried out during the process of Preimplantation Genetic Testing (PGT).

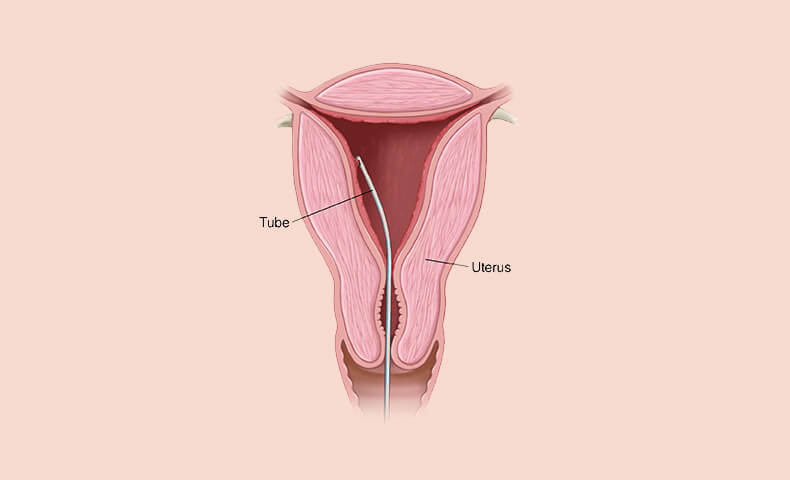
During the ICSI cycle, a few cells called Trophoblast cells are removed (biopsied) from the Day 5 / Day 6 embryo and are checked for genetic abnormalities.
The embryos, that are reported normal, are then transferred to the mother’s uterus.
It is carried out for couples who are at a high risk for various genetic disorders, those with male factor, in advancing maternal age or repeated failed IVF.

This is a test that helps to assess the personalised window of implantation for each patient by evaluating the endometrial receptivity It analyses the presence of 248 specific genes using NGS (next generation sequencing)
Useful in cases of :
Recurrent implantation failure
Atrophic or hypertrophic endometrium

Useful in cases with recurrent thin endometrium.
Improves the pregnancy rates in women with recurrent implantation failure, thin endometrium
